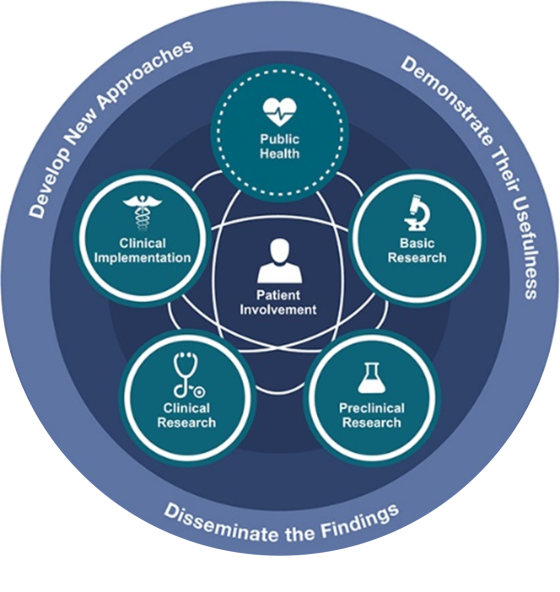
Translational Research is a commonly used term in medical research which explains how researchers ‘translate’ basic science discoveries from the laboratory into clinical application. The purpose of this research is to improve how we prevent and diagnose health conditions, discover new treatments, and improve the way we help patients for better outcomes. Health and medical research is more likely to be translated into practice and have greater real-world impact when it responds to locally prioritised needs and is shaped by the people who will use and benefit from the research.
Translational research accelerates innovation in healthcare. Implementation of the new knowledge highlighting new methods in clinical best practice published in journals, guidelines and government reports delivers benefit to patients.
Policy communication and advocacy have a large part to play in ensuring that such research has its desired impact on society. In other instances, a technology solution may be the route to address a particular problem. This is where internal innovation generating new intellectual property and collaboration with industry has a large part to play in converting new inventions into life-improving products serving patients’ needs.
Our research focus areas: big data; biomedical science; childhood cancer; mental health and neurosciences; next-generation technologies, imaging, and precision medicine; and virtual care research translated to excellence in clinical care.
We aspire to:
- Deliver person-centred research (and subsequent care) by putting people and their families at the centre of decisions, planning and development. Creating equal partnerships and improving the way professionals and patients think about care and their relationships. Making the experience as important as the outcome. Ensuring people are involved in- and central to- their care is now recognised as a key component of developing high quality healthcare.
- Undertake holistic research that investigates the impact of education, the natural and built environment, lifestyle and social-economic factors, and social networks on wellbeing in our communities. We will use this knowledge to produce innovative interventions in health.
- Incorporate data generated from routine clinical care and record-keeping with novel information platforms to enhance diagnosis, treatment and evaluation, and lead to new discoveries.
- Lead innovation in health and wellness, care and delivery, treatment and diagnostics. Focusing on less-invasive treatments and procedures, harnessing creativity and technology, reducing cost, increasing collaboration across and outside of RHIP, supporting ideas pipeline and keeping patients out of hospitals.
For more information on translational research at RHIP, please contact:
Celia Loneragan
Translational Research Lead
celia.loneragan@unsw.edu.au